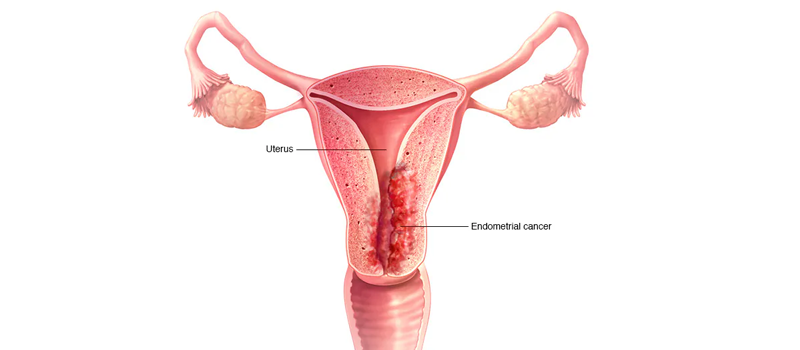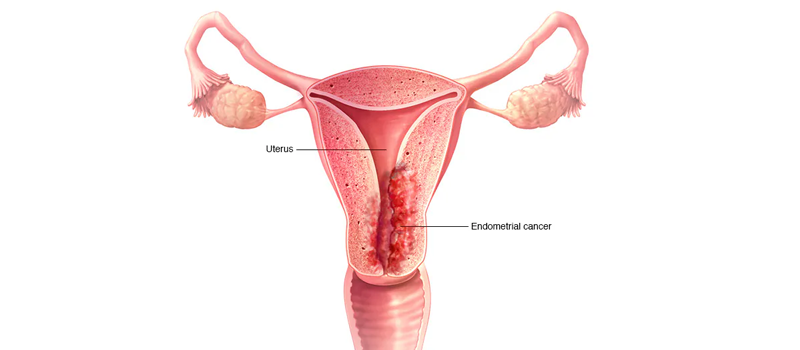
Uterine Cancer: Understanding, Diagnosis, and Treatment
Uterine cancer, also known as endometrial cancer, originates in the lining of the uterus (endometrium) and is the most common gynecologic cancer in women. While uterine cancer predominantly affects postmenopausal women, it can occur at any age. Understanding the risk factors, symptoms, and treatment options for uterine cancer is essential for early detection and improved outcomes.
Understanding Uterine Cancer:
Uterine cancer develops when cells in the endometrium undergo abnormal changes and grow out of control, forming a tumor. The exact cause of uterine cancer is not fully understood, but certain factors may increase the risk, including:
- Hormonal imbalances: Excessive estrogen without progesterone balance, such as in women who have never been pregnant or have a history of irregular menstrual cycles, may increase the risk.
- Obesity: Obesity is strongly associated with an increased risk of uterine cancer, as fat tissue can produce estrogen.
- Age: Uterine cancer is more common in older women, particularly those who have gone through menopause.
- Hormone therapy: Prolonged use of estrogen-alone hormone replacement therapy without progesterone after menopause may increase the risk.
- Family history: A family history of uterine or ovarian cancer may predispose an individual to developing uterine cancer.
Symptoms and Diagnosis:
Early-stage uterine cancer may present with symptoms, including abnormal vaginal bleeding (especially after menopause), pelvic pain or discomfort, pain during intercourse, and abnormal vaginal discharge. However, some women with uterine cancer may not experience noticeable symptoms until the disease has progressed.
Diagnostic tests for uterine cancer include:
- Transvaginal ultrasound: This imaging test uses sound waves to create pictures of the uterus and may help identify abnormalities, such as thickened endometrial lining.
- Endometrial biopsy: During this procedure, a sample of tissue from the lining of the uterus is collected and examined under a microscope to check for cancer cells.
- Hysteroscopy: A thin, lighted tube with a camera (hysteroscope) is inserted through the vagina and cervix into the uterus to visually inspect the uterine lining and collect tissue samples if necessary.
Treatment Options:
Treatment for uterine cancer depends on several factors, including the stage and grade of the cancer, the patient's overall health, and their preferences. Treatment options may include:
- Surgery: Surgery is the primary treatment for uterine cancer and typically involves removing the uterus (hysterectomy) and sometimes the fallopian tubes and ovaries. Lymph nodes may also be removed to check for cancer spread.
- Radiation therapy: Radiation therapy uses high-energy beams to kill cancer cells and may be used before or after surgery to destroy any remaining cancer cells or reduce the risk of recurrence.
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells or stop them from growing and may be used alone or in combination with surgery and/or radiation therapy, particularly in advanced or recurrent cases.
Prognosis and Outlook:
The prognosis for uterine cancer depends on factors such as the stage and grade of the cancer, the patient's age and overall health, and their response to treatment. Early detection and treatment offer the best chance for favorable outcomes, with high survival rates for localized disease.
Conclusion:
Uterine cancer is a significant health concern for women, but advancements in early detection methods, treatment options, and supportive care have improved outcomes and quality of life for many patients. By understanding the risk factors, recognizing symptoms, and seeking prompt medical attention, women can take proactive steps towards early detection and successful treatment of uterine cancer. Regular gynecologic exams and screenings are essential for maintaining women's health and detecting uterine cancer at its earliest stages.